written by Jill Neimark
written by Jill Neimark
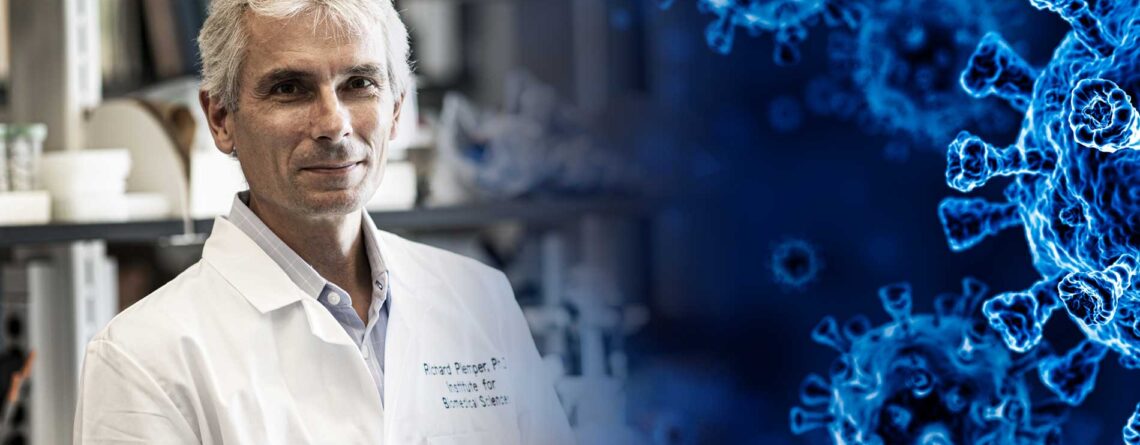
Viruses have an amazing capacity to mutate. But what if we could turn that against them? Richard Plemper, professor in the Institute for Biomedical Sciences, is working to exploit this rapid evolution.
Richard Plemper loves to run, and his dogs know it. In the dawn of a Georgia morning both his Airedale terrier Ludo and retriever Sirius, named by his daughter after the Harry Potter characters, wait eagerly by the front door of the Decatur home where Plemper and his wife and three children live. The silver-haired cell biologist lets them out onto the wraparound porch and they bound ahead, happily running with him as he winds along the hilly, tree-lined streets of Decatur. It’s a good way to clear his mind for another day dedicated to conquering the deadly viruses that plague humans, from measles to influenza to the novel coronavirus that has killed more than a half million Americans in the past year.
“Viruses are our teachers,” says Plemper, a German-born scientist who is a professor at Georgia State University’s Institute for Biomedical Sciences. “So much of what we have learned about how our own cells function comes from studying how viruses exploit cellular systems and defense strategies.”
Even when tamed by our immune system, viruses prove to be amazing escape artists, mutating and recombining to create new versions of themselves. (The reason we need to get flu vaccines every year is because influenza viruses evolve quickly and the duration of immunity is short.) Rapid mutation is a hallmark of many viruses — one we all witnessed in action this past winter and spring when SARS-CoV-2, the virus that causes COVID-19, evolved and similar mutations emerged in different countries simultaneously. Those mutations led to variants that were much more transmissible and possibly less susceptible to our immune system’s antibodies than the first strains of the virus. They were different enough in Brazil to re-infect citizens who had already had COVID-19.
But what if we could harness this propensity for mutation and turn it against the virus? What if we could invent a small molecule — a drug — that tricks viruses into mutating so ferociously they actually die? And what if we could do it in such a way the virus couldn’t outwit our drugs — could not easily become resistant to them?
Plemper and his colleagues have done just that. They have characterized small molecules that essentially mutate a virus to death. By intersecting with the virus at key hinge points in its replication machinery, these new molecules can trick the pathogen into churning out reproduction errors until it essentially collapses.
Plemper says a new class of antiviral drugs could be the perfect complement to global vaccination strategies. Vaccines, which he strongly supports, are not enough to meet the challenges that new pandemics and persistent pathogens pose to humans in our global, interconnected society. Even with the unprecedented speed of vaccine development for COVID-19, says Plemper, we cannot stop a mounting pandemic caused by a newly emerged virus through vaccination alone. We need an arsenal of broadly active antiviral drugs as an immediately available first-line defense.
Anthony Fauci, chief of the National Institute of Allergy and Infectious Diseases, agrees.
“The bottom line of what we need to do looking forward, and the clear need in this, is the development of potent antivirals directly acting on SARS-CoV-2,” Fauci said at a White House briefing this winter. “Antivirals would revolutionize the fight against SARS-CoV-2, since they block viruses from replicating and can stop people from getting very sick or dying.”
The past year of the pandemic has been, says Plemper, one of the most challenging and exciting in his career.
“My colleagues and I have trained for the moment of such a crisis through two decades dedicated to the identification and development of antiviral therapeutics,” he explains. Now they find themselves stepping up to meet history. “I believe we can bring forward what we know and make a genuine contribution.”
We cannot stop a mounting pandemic caused by a newly emerged virus through vaccination alone. We need an arsenal of broadly active antiviral drugs as an immediately available first-line defense.
We cannot stop a mounting pandemic caused by a newly emerged virus through vaccination alone. We need an arsenal of broadly active antiviral drugs as an immediately available first-line defense.
In 1999, when Plemper first arrived at Minnesota’s Mayo Clinic as a postdoctoral researcher, he decided to study measles (Morbillivirus) virus. Measles is so contagious it sickens an astounding nine of 10 people exposed, and a measles carrier can infect others up to four days before a rash first appears. Most of measles’ victims are children, and before widespread vaccination, measles routinely killed a million people a year. Even with vaccination, measles still causes 100,000 deaths annually, with outbreaks around the world, including an outbreak in 31 U.S. states in 2019.
The measles virus genome is composed of negative polarity RNA (ribonucleic acid) strands and the virus is a member of the paramyxovirus family, which also includes parainfluenza viruses and mumps virus — pathogens that tend to target mostly children. To develop effective antivirals for measles, Plemper first needed to understand the virus at the molecular level.
“Viruses have a very complex protein machinery with many moving parts,” he explains.
He began to analyze the virus’s structure, focusing in particular on its densely packed glycoproteins, molecules made of sugars and proteins that live on the outer membrane of the virus, and the viral polymerase complex, which plays a critical role in virus replication. He wanted to know how glycoproteins on the virus’ membrane fused with the membranes of a cell, how the virus then manages to enter the cell’s interior and how it effectively replicates its genome. He was looking for critical hinge points in viral function, aspects of its machinery that were so essential that interrupting them could prevent the entire system from running. If they were that essential, they might be broadly conserved across a number of different viral pathogens in that family. That would allow him to develop broad-spectrum drugs that targeted whole classes of pathogens and not just one disease.
He had another requirement as well: the compound must be orally bioavailable, meaning it can be taken by mouth and therefore started early after infection. The drug also must be well tolerated. This is particularly critical in medicines given to children. The medicines must be exceptionally safe.
So he set about studying measles, using electron microscopes to examine its subterranean world of spikes, rings and tubular structures, and learning how these shifted during its life cycle.
“Richard is very good at studying protein structures and is passionately intense in his studies of viruses. At times he had to go to extra lengths to justify his stellar work on measles, largely because disease caused by measles is not a big threat in the United States,” recalls Paul Spearman, the Albert B. Sabin professor and director of Infectious Diseases at Cincinnati Children’s Hospital Medical Center.
(When Spearman was division chief for infectious diseases at Emory University, he had recruited Plemper as a young assistant professor).
“However, it turns out working on measles is important for a number of reasons,” he says. “Measles virus can teach us a lot about how viruses function in ways that are applicable to the study of other viruses. Measles also remains an important public health threat globally, so antivirals against measles are very much needed.”
Plemper also did something else that reflected his ability to plan ahead. He began to assemble a library of small molecules and established an automated facility in his lab that would allow him to quickly screen for activity against many viruses.
“This was the beginning of a great intellectual journey,” explains his colleague Benhur Lee, professor of microbiology at the Icahn School of Medicine at Mount Sinai.
Lee calls himself the “virus whisperer’” and has coauthored papers with Plemper. Some molecules in the screens, for instance, turned out to be pan-reactive, inhibiting almost everything, which could be toxic to human cells. Plemper methodically deleted all non-developable pan-reactive molecules and began to curate a large library of drug-like molecules that might one day be used to create antiviral drugs. It was methodical, obsessive work that took several years to complete.
“It was Richard’s years of optimization and work on this library of molecules that laid the groundwork for today’s successes,” says Lee.
By 2018, Plemper and his team had discovered a novel drug target unique to the viral polymerase that was critical for the replication of the measles virus. With this new understanding, he could begin to zero in on possible therapeutics. In 2020, the team announced the discovery of a broad spectrum, oral drug that could target many different paramyxoviruses.
Arriving at the discovery was not easy — in total, they tested 141,936 different compounds in the laboratory. The new compound, called GHP88309, is able to bind to and inhibit paramyxovirus polymerases, which are protein complexes essential to viral replication. This means it could likely treat not only measles, but also parainfluenza viruses and related paramyxoviruses of the henipavirus group, which are usually found in Australia and Asia and can cause fatal encephalitis. There is no approved treatment option some of these viruses today.
To test the compound, they first studied its impact on measles-infected human organoid lung tissue. Organoids are three-dimensional tissue cultures that are derived from stem cells. They can be designed to act much like an organ or simply to produce certain types of cells. Plemper and his team designed tissue that recreated the lining of the lungs, known as the epithelium. By testing it in this tissue they could verify its activity, potency and safety. The compound was found to be highly potent, with very low toxicity, in this lung tissue. It broadly inhibited measles, parainfluenza viruses and other viruses.
Then they tested it in animals, where it led to complete recovery from a lethal paramyxovirus infection — human parainfluenza virus type 3 (HPIV3).
“Every year, up to 14 percent of adults who get stem cell transplants in the United States suffer from life-threatening HPIV3 infections,” says Plemper. The research team’s work was published in the prestigious journal Nature Microbiology. GHP88309 is undergoing rigorous testing for safety and Plemper is working with the university’s Office of Technology Transfer and Commercialization to help advance it toward the clinic. The road ahead is long but based on the exciting results the group has obtained, Plemper expects the compound will advance to clinical trials in human patients.
By assembling a library of small molecules and establishing an automated facility in his lab, Plemper can quickly screen for activity against many viruses.
By assembling a library of small molecules and establishing an automated facility in his lab, Plemper can quickly screen for activity against many viruses.
An even more pressing challenge lay ahead: As the COVID-19 pandemic gained pace in early 2020, Plemper and his team at Georgia State immediately began thinking of their set of antiviral candidates, and whether any may have activity against SARS-COV-2, the virus that caused the pandemic, which had killed more than 2.5 million people worldwide by March 2021. In collaboration with Emory University’s nonprofit Drug Innovation Ventures at Emory (DRIVE), Plemper had worked on an antiviral called molnupiravir (originally referred to as EIDD-2801 in studies). His lab had just reported its effectiveness against influenza in a publication in Science Translational Medicine when SARS-CoV-2 emerged. In a matter of weeks, they quickly shifted to test the molecule against this novel coronavirus and found it crippled the virus in infected animals, stopping it from replicating in a mere 24 hours.
Influenza and SARS-Cov-2 are RNA viruses, and Plemper says the drug exploits a key vulnerability in these types of pathogens — the fact that they evolve rapidly, generating mutations as they change, and thus “live genetically close to the edge.”
Too many random mutations in a short time will lead the virus into what’s known as “error catastrophe,” rendering it nonfunctional. The term was first coined in the 1970s and it’s thought that some broad-spectrum antiviral drugs — such as ribavirin, which treats hepatitis C — work by increasing mutations in the virus, leading to error catastrophe and collapse.
Molnupiravir works by tricking the virus, causing it to make wrong base pairings that lead to a large number of mutations in the viral genome. The new virions incorporating these mutated genomes simply cannot function.
Humans aren’t the only mammal vulnerable to SARS-Cov-2. It has also been found to infect minks and ferrets, for example. Though ferrets easily contract and pass on the infection, they tend to have a mostly asymptomatic or relatively mild course of illness. In that way, says Plemper, their infection resembles that of most younger adults. In a study on ferrets infected with the SARS-Cov-2 — and with a high viral load in their nasal tissues and secretions — treatment twice a day with molnupiravir completely suppressed spread of the virus to other, untreated ferrets.
Molnupiravir is now in two randomized, double-blind, placebo-controlled Phase II trials in humans to test optimal dosage and efficacy — one study with 80 recently hospitalized participants and the other with 204 outpatients. No formal results have been reported yet, but a first assessment released at the beginning of March demonstrated the drug efficiently reduces viral burden in human patients.
Plemper says so far in lab experiments, viruses vulnerable to the drug have not developed resistance.
“This molecule’s barrier to resistance is unusually high,” he says.
This means it may be equally effective against new variants of the novel coronavirus that have recently emerged or may emerge in the future. Plemper does note that drugs that enhance mutagenesis and errors in viruses can cause mutations in human cells as well, but so far molnupiravir has proven safe and was well-tolerated without mutagenic effects on the host. The compound is also effective against two earlier coronaviruses — MERS, and SARS-CoV, which killed nearly 800 Americans in 2003.
The great advantage of an effective, broad-spectrum oral drug is that it can be taken early in the course of disease like COVID-19, before a patient develops severe symptoms. If the human studies prove as successful as the animal studies, COVID-19 patients treated with molnupiravir could become non-infectious within 24 to 36 hours — protecting themselves as well as others around them.
“The biggest take-home message for me personally,” says Plemper, “is that we should always start by asking ourselves, ‘What do the patients need?’ Don’t start with a molecule that you may like, start with the patients and their needs. They define the necessary properties a successful drug must have. Since that was our endpoint, we designed assays that had a high chance to meet that objective.”
“We should always start by asking ourselves, ‘What do the patients need?’ Don’t start with a molecule that you may like, start with the patients and their needs.”
“We should always start by asking ourselves, ‘What do the patients need?’ Don’t start with a molecule that you may like, start with the patients and their needs.”
There seem to be more viruses than there are stars in the universe, and scientists have identified several hundred of them that infect humans. Developing drugs against any one of these viruses can be a long and arduous process. However, it can be made faster and less tedious through collaboration, says Plemper. His lab continues to work closely with Emory, and many of their published papers are co-authored with top cell biologists at major institutions and universities.
“You cannot do it without experts in every area,” he says. “It truly takes a village. You need people with expertise in virology, in biochemistry, in synthetic chemistry, pharmacology and more.”
Plemper says his decades of work on viruses have only deepened his fascination with them.
“They have been exposed to all of our defense strategies,” he says, “and the viruses that persist are really brilliantly selected by evolution. From an engineering perspective it is amazing how a virus manages to survive in spite of the fact that its host makes a major effort to kill it.”
Viruses are, says this cell biologist, great cell biologists themselves, and we have much to learn from them.









Leave a Reply