SPRING 2018 ISSUE >>
[post-fields post_field=”wpcf-byline”][easy-social-share buttons=”facebook,twitter,linkedin”] HILE HIKING IN THE WOODS, YOU FEEL A SCRATCH AS YOUR LEG GRAZES A FALLEN TREE LIMB. BY THE TIME YOU MAKE IT HOME, THE SCRATCH IS RED, SWOLLEN AND TENDER TO THE TOUCH. THAT’S THE RESULT OF INFLAMMATION, WHICH OCCURS WHEN A RUSH OF WHITE BLOOD CELLS IS MOBILIZED BY YOUR BODY AS A FIRST LINE OF DEFENSE AGAINST INFECTION OR INJURY.
HILE HIKING IN THE WOODS, YOU FEEL A SCRATCH AS YOUR LEG GRAZES A FALLEN TREE LIMB. BY THE TIME YOU MAKE IT HOME, THE SCRATCH IS RED, SWOLLEN AND TENDER TO THE TOUCH. THAT’S THE RESULT OF INFLAMMATION, WHICH OCCURS WHEN A RUSH OF WHITE BLOOD CELLS IS MOBILIZED BY YOUR BODY AS A FIRST LINE OF DEFENSE AGAINST INFECTION OR INJURY.
 HILE HIKING IN THE WOODS, YOU FEEL A SCRATCH AS YOUR LEG GRAZES A FALLEN TREE LIMB. BY THE TIME YOU MAKE IT HOME, THE SCRATCH IS RED, SWOLLEN AND TENDER TO THE TOUCH. THAT’S THE RESULT OF INFLAMMATION, WHICH OCCURS WHEN A RUSH OF WHITE BLOOD CELLS IS MOBILIZED BY YOUR BODY AS A FIRST LINE OF DEFENSE AGAINST INFECTION OR INJURY.
HILE HIKING IN THE WOODS, YOU FEEL A SCRATCH AS YOUR LEG GRAZES A FALLEN TREE LIMB. BY THE TIME YOU MAKE IT HOME, THE SCRATCH IS RED, SWOLLEN AND TENDER TO THE TOUCH. THAT’S THE RESULT OF INFLAMMATION, WHICH OCCURS WHEN A RUSH OF WHITE BLOOD CELLS IS MOBILIZED BY YOUR BODY AS A FIRST LINE OF DEFENSE AGAINST INFECTION OR INJURY.
Without the immune system, humans would fall victim to any virus, bacteria or germ they face, says Jian-Dong Li, director of the Institute for Biomedical Sciences and a Georgia Research Alliance Eminent Scholar in inflammation and immunity. And inflammation is one of the biggest weapons in your immune arsenal.
“It is a natural response that’s required to keep us healthy,” says Li.
Under normal circumstances, inflammation is short-lived. A few days later, the cut heals, the redness fades and the swelling diminishes. Yet “there can be too much of a good thing,” says Li. If the immune response doesn’t subside, the body can remain in a state of simmering inflammation for months or even years.
Chronic inflammation isn’t something you can feel, like a swollen, throbbing scratch. Instead, it’s more like a silent, slow burn — one with a profound impact on the body. Research shows runaway inflammation can damage healthy tissue, feed tumors and leave the door open for illness and disease. It’s a hallmark of most chronic diseases and of some of the leading causes of death in the United States, including neurological disorders, cardiovascular disease, pulmonary diseases, cancer and obesity.
But how exactly is inflammation involved? Does it cause these diseases or simply make them worse? Scientists across Georgia State University are working to better understand the relationship between chronic inflammation and a number of serious health conditions. They’re also striving to uncover what fuels uncontrolled inflammation and pinpoint ways to prevent the body’s inflammatory response from going awry.
Without the immune system, humans would fall victim to any virus, bacteria or germ they face, says Jian-Dong Li, director of the Institute for Biomedical Sciences and a Georgia Research Alliance Eminent Scholar in inflammation and immunity. And inflammation is one of the biggest weapons in your immune arsenal.
“It is a natural response that’s required to keep us healthy,” says Li.
Under normal circumstances, inflammation is short-lived. A few days later, the cut heals, the redness fades and the swelling diminishes. Yet “there can be too much of a good thing,” says Li. If the immune response doesn’t subside, the body can remain in a state of simmering inflammation for months or even years.
Chronic inflammation isn’t something you can feel, like a swollen, throbbing scratch. Instead, it’s more like a silent, slow burn — one with a profound impact on the body. Research shows runaway inflammation can damage healthy tissue, feed tumors and leave the door open for illness and disease. It’s a hallmark of most chronic diseases and of some of the leading causes of death in the United States, including neurological disorders, cardiovascular disease, pulmonary diseases, cancer and obesity.
But how exactly is inflammation involved? Does it cause these diseases or simply make them worse? Scientists across Georgia State University are working to better understand the relationship between chronic inflammation and a number of serious health conditions. They’re also striving to uncover what fuels uncontrolled inflammation and pinpoint ways to prevent the body’s inflammatory response from going awry.
When Inflammation Goes Wrong
If some inflammation is a good thing, while too much is bad, then how does the body strike the right balance? Although the mechanisms behind chronic inflammation are not fully understood, scientists do know your genes are partially responsible for regulating the immune response, acting as built-in brakes to halt inflammation after it has served its purpose.
For example, Georgia State researchers have found that a gene known as CYLD can curb certain types of inflammation. If the body’s inflammatory immune response continues unchecked, as if the brakes have been cut, an underactive CYLD gene may be to blame.
For those with defective genes, how can outof-control inflammation be stopped? That’s a puzzle researchers at the Center for Inflammation, Immunity & Infection, housed in the Institute for Biomedical Sciences, are trying to solve. Antiinflammatory medications are effective, but they can also shut down the inflammatory response entirely, essentially pulling the plug on the body’s whole immune system.
Li and his colleagues hope to develop a drug that would improve the function of CYLD, prompting it to tap the brakes on inflammation at just the right time. They are also working to identify other genes that may contribute to chronic inflammation.
“The idea is that we could adjust the dose based on exactly how much we want to tamp down inflammation,” says Li. “And we could do it with fewer side effects than existing antiinflammatory drugs.”
When Inflammation Goes Wrong
If some inflammation is a good thing, while too much is bad, then how does the body strike the right balance? Although the mechanisms behind chronic inflammation are not fully understood, scientists do know your genes are partially responsible for regulating the immune response, acting as built-in brakes to halt inflammation after it has served its purpose.
For example, Georgia State researchers have found that a gene known as CYLD can curb certain types of inflammation. If the body’s inflammatory immune response continues unchecked, as if the brakes have been cut, an underactive CYLD gene may be to blame.
For those with defective genes, how can outof-control inflammation be stopped? That’s a puzzle researchers at the Center for Inflammation, Immunity & Infection, housed in the Institute for Biomedical Sciences, are trying to solve. Antiinflammatory medications are effective, but they can also shut down the inflammatory response entirely, essentially pulling the plug on the body’s whole immune system.
Li and his colleagues hope to develop a drug that would improve the function of CYLD, prompting it to tap the brakes on inflammation at just the right time. They are also working to identify other genes that may contribute to chronic inflammation.
“The idea is that we could adjust the dose based on exactly how much we want to tamp down inflammation,” says Li. “And we could do it with fewer side effects than existing antiinflammatory drugs.”
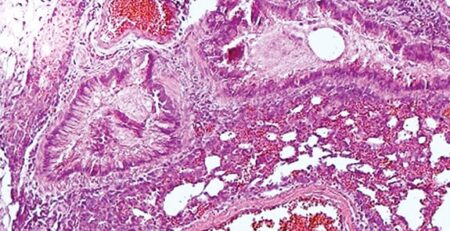
Georgia State researchers are also studying the environmental and lifestyle factors that can provoke prolonged, systemic inflammation. One of those factors may be components of a typical Western diet. Additives called emulsifiers give processed foods such as ice cream and yogurt their smooth, creamy texture, and prevent peanuts and oil from separating in peanut butter. Yet according to studies led by Benoit Chassaing, assistant professor in the Institute for Biomedical Sciences, and Andrew Gewirtz, professor in the Center for Inflammation, Immunity & Infection, emulsifiers also alter the makeup of bacteria in the gut, making it easier for those bacteria to break through the protective layer of mucus lining the intestines. If the bacteria reach the intestinal wall — which is normally sterile — and trigger an immune response, that can lead to chronic inflammation.
In the study, the researchers found an emulsifier-supplemented diet dramatically increased the risk of colitis — a form of chronic inflammation similar to inflammatory bowel disease (IBD) in humans — among mice who were genetically predisposed to develop the disorder. Genetically typical mice who were fed emulsifiers developed low-grade intestinal inflammation along with increased body fat, increased food intake and higher blood sugar levels — all early signs of obesity, diabetes and other metabolic problems. The feces of the emulsifier-fed mice also contained higher levels of a bacteria that can penetrate the intestines’ protective mucus and higher levels of proinflammatory bacteria in general.
Chassaing and Gewirtz are now putting together a clinical trial in partnership with the University of Pennsylvania to study the effects of emulsifiers on human gut bacteria. But Chassaing is not waiting for the results to make changes in his own diet. He sees a direct correlation between skyrocketing rates of IBD in the U.S. and our everincreasing consumption of processed foods.
To avoid emulsifiers, Chassaing and his family prepare meals from whole, raw ingredients such as fresh meats and vegetables, and buy natural peanut butter you have to stir yourself.
“And,” he notes, “you can buy emulsifier-free ice cream.”
Georgia State researchers are also studying the environmental and lifestyle factors that can provoke prolonged, systemic inflammation. One of those factors may be components of a typical Western diet. Additives called emulsifiers give processed foods such as ice cream and yogurt their smooth, creamy texture, and prevent peanuts and oil from separating in peanut butter. Yet according to studies led by Benoit Chassaing, assistant professor in the Institute for Biomedical Sciences, and Andrew Gewirtz, professor in the Center for Inflammation, Immunity & Infection, emulsifiers also alter the makeup of bacteria in the gut, making it easier for those bacteria to break through the protective layer of mucus lining the intestines. If the bacteria reach the intestinal wall — which is normally sterile — and trigger an immune response, that can lead to chronic inflammation.
In the study, the researchers found an emulsifier-supplemented diet dramatically increased the risk of colitis — a form of chronic inflammation similar to inflammatory bowel disease (IBD) in humans — among mice who were genetically predisposed to develop the disorder. Genetically typical mice who were fed emulsifiers developed low-grade intestinal inflammation along with increased body fat, increased food intake and higher blood sugar levels — all early signs of obesity, diabetes and other metabolic problems. The feces of the emulsifier-fed mice also contained higher levels of a bacteria that can penetrate the intestines’ protective mucus and higher levels of proinflammatory bacteria in general.
Chassaing and Gewirtz are now putting together a clinical trial in partnership with the University of Pennsylvania to study the effects of emulsifiers on human gut bacteria. But Chassaing is not waiting for the results to make changes in his own diet. He sees a direct correlation between skyrocketing rates of IBD in the U.S. and our everincreasing consumption of processed foods.
To avoid emulsifiers, Chassaing and his family prepare meals from whole, raw ingredients such as fresh meats and vegetables, and buy natural peanut butter you have to stir yourself.
“And,” he notes, “you can buy emulsifier-free ice cream.”
INFLAMED IN THE BRAIN
In recent years, scientists have come to discover that neuroinflammation, or inflammation in the brain, plays an important role in triggering obesity, high blood pressure and high cholesterol — factors that can lead to conditions like heart disease, diabetes and stroke. Georgia State’s new Center for Neuroinflammation & Cardiometabolic Diseases seeks to uncover the mechanisms that set off neuroinflammation and determine how exactly it contributes to these health issues.
Their work may help explain the links between seemingly disconnected conditions. High blood pressure, for example, is a known risk factor for Alzheimer’s disease.
“We once thought these disorders were unrelated,” says Javier Stern, professor of neuroscience and founding director of the center. “Now we want to determine whether the same inflammatory process that we see in cardiovascular and metabolic disorders can also trigger neuropsychiatric and mood disorders.”
They’re doing it by eavesdropping on the brain. The inflammatory response involves communication among different brain cells, so Stern and his colleagues are learning more about the process by listening in on those conversations.
Neurons generate electrical signals when they communicate with each other, while glial cells leave traces of their communication via changes in calcium levels in the brain. Georgia State scientists are combining electrophysiological approaches to wiretap the communications between the various cells, recording neurons’ electrical signals and using sophisticated imaging techniques to monitor calcium changes brought about by glial cells.
“We believe this feedback between the cells creates the setting for neuroinflammation,” says Stern.
At the same time, he adds, in a brain that’s already inflamed, brain cells are compromised, which affects the way they communicate. “It’s a cascading effect in which one thing goes wrong, and that makes another thing get even worse,” Stern says.
Stern hopes that pinpointing when and why communication between brain cells runs amok will allow him and his team develop a treatment that intercepts that exact moment when the inflammatory process begins.
Inflammation in
the brain, plays
an important
role in triggering
obesity, high blood
pressure and high
cholesterol —
factors that can
lead to conditions
like heart disease,
diabetes and
stroke.
INFLAMED IN THE BRAIN
In recent years, scientists have come to discover that neuroinflammation, or inflammation in the brain, plays an important role in triggering obesity, high blood pressure and high cholesterol — factors that can lead to conditions like heart disease, diabetes and stroke. Georgia State’s new Center for Neuroinflammation & Cardiometabolic Diseases seeks to uncover the mechanisms that set off neuroinflammation and determine how exactly it contributes to these health issues.
Their work may help explain the links between seemingly disconnected conditions. High blood pressure, for example, is a known risk factor for Alzheimer’s disease.
“We once thought these disorders were unrelated,” says Javier Stern, professor of neuroscience and founding director of the center. “Now we want to determine whether the same inflammatory process that we see in cardiovascular and metabolic disorders can also trigger neuropsychiatric and mood disorders.”
They’re doing it by eavesdropping on the brain. The inflammatory response involves communication among different brain cells, so Stern and his colleagues are learning more about the process by listening in on those conversations.
Neurons generate electrical signals when they communicate with each other, while glial cells leave traces of their communication via changes in calcium levels in the brain. Georgia State scientists are combining electrophysiological approaches to wiretap the communications between the various cells, recording neurons’ electrical signals and using sophisticated imaging techniques to monitor calcium changes brought about by glial cells.
“We believe this feedback between the cells creates the setting for neuroinflammation,” says Stern.
At the same time, he adds, in a brain that’s already inflamed, brain cells are compromised, which affects the way they communicate. “It’s a cascading effect in which one thing goes wrong, and that makes another thing get even worse,” Stern says.
Stern hopes that pinpointing when and why communication between brain cells runs amok will allow him and his team develop a treatment that intercepts that exact moment when the inflammatory process begins.
Inflammation in
the brain, plays
an important
role in triggering
obesity, high blood
pressure and high
cholesterol —
factors that can
lead to conditions
like heart disease,
diabetes and
stroke.
Additives called emulsifiers are what give processed foods like ice cream and yogurt their smooth, creamy texture. Yet according to studies led by Georgia State, they also alter the makeup of bacteria in the gut, which can lead to chronic inflammation.
Additives called emulsifiers are what give processed foods like ice cream and yogurt their smooth, creamy texture. Yet according to studies led by Georgia State, they also alter the makeup of bacteria in the gut, which can lead to chronic inflammation.
Extinguishing the Fire Inside
As research has revealed the connection between inflammation and many major diseases, scientists have been working to identify compounds that can tamp down or block the overactive immune response. Certain types of dietary fiber may prove to be potent anti-inflammatory agents, according to Gewirtz. A study he published with colleagues in Cell Host and Microbe found that inulin — a type of fiber found in asparagus, onions, bananas, sprouted wheat and garlic — may prevent metabolic problems caused by a high-fat diet by increasing the body’s production of interleukin-22, an immune protein that regulates inflammation.
For mice whose healthy gut bacteria had been depleted by a fatty diet, adding inulin to their diet restored their good bacteria. The fiber also re-established a healthy separation between gut bacteria and the intestinal wall. Gewirtz says this points to the possibility of creating an antiinflammatory drug containing interleukin-22.
“For people who aren’t willing to change their diets, it may be possible to administer this protein pharmacologically to help prevent chronic inflammatory diseases,” he says.
Time to
Get Your
Inflammation
Checked?
Chronic inflammation is now known to drive many life-threatening diseases, yet it remains difficult to diagnose. High blood levels of C-reactive protein, a molecule produced by the liver in response to inflammation, could be a good indicator of prolonged systemic inflammation, but more sensitive tests are needed to distinguish among different types of inflammation related to various disease states. Research at the Center for Diagnostics & Therapeutics seeks to identify indicators of inflammation specific to IBD.
“Currently, the biomarkers lack specificity and, used alone, don’t hold much value,” says Emilie Viennois, a postdoctoral researcher at the center.
Identifying new biomarkers could allow doctors to distinguish more quickly between Crohn’s disease and ulcerative colitis — two different forms of IBD — and help determine which medication would be most effective. Viennois is searching for new biomarkers in microRNA, molecules that play a key role in regulating gene activity.
Extinguishing the Fire Inside
As research has revealed the connection between inflammation and many major diseases, scientists have been working to identify compounds that can tamp down or block the overactive immune response. Certain types of dietary fiber may prove to be potent anti-inflammatory agents, according to Gewirtz. A study he published with colleagues in Cell Host and Microbe found that inulin — a type of fiber found in asparagus, onions, bananas, sprouted wheat and garlic — may prevent metabolic problems caused by a high-fat diet by increasing the body’s production of interleukin-22, an immune protein that regulates inflammation.
For mice whose healthy gut bacteria had been depleted by a fatty diet, adding inulin to their diet restored their good bacteria. The fiber also re-established a healthy separation between gut bacteria and the intestinal wall. Gewirtz says this points to the possibility of creating an antiinflammatory drug containing interleukin-22.
“For people who aren’t willing to change their diets, it may be possible to administer this protein pharmacologically to help prevent chronic inflammatory diseases,” he says.
Time to Get Your Inflammation Checked?
Chronic inflammation is now known to drive many life-threatening diseases, yet it remains difficult to diagnose. High blood levels of C-reactive protein, a molecule produced by the liver in response to inflammation, could be a good indicator of prolonged systemic inflammation, but more sensitive tests are needed to distinguish among different types of inflammation related to various disease states. Research at the Center for Diagnostics & Therapeutics seeks to identify indicators of inflammation specific to IBD.
“Currently, the biomarkers lack specificity and, used alone, don’t hold much value,” says Emilie Viennois, a postdoctoral researcher at the center.
Identifying new biomarkers could allow doctors to distinguish more quickly between Crohn’s disease and ulcerative colitis — two different forms of IBD — and help determine which medication would be most effective. Viennois is searching for new biomarkers in microRNA, molecules that play a key role in regulating gene activity.
Gewirtz is also working with Chassaing to explore the potential for a vaccine that could inoculate the gut against the havoc caused by a poor diet.
Didier Merlin, professor in the Institute for Biomedical Sciences and a Research Career Scientist at Veteran Affairs Medical Center, is investigating whether a common supermarket ingredient — ginger — could help combat inflammation involved in IBD and colitis-associated colon cancer. A team of researchers led by Merlin is developing ginger-derived nanoparticles to deliver the ingredient’s anti-inflammatory compounds directly to the site of the inflammation.
“It’s a novel, nontoxic delivery system to treat inflamed intestinal tissue,” says Lewins Walter, a Ph.D. candidate and researcher in Merlin’s lab.
“We’re looking at these nanoparticles as a natural remedy for IBD.”
Still, Li notes that overactive inflammation is a complex process with many causes, and finding a solution will require a multipronged approach.
“It won’t be neuroscience or microbiology — or any single science — that will rein in the burden of inflammation or chronic disease,” he says. “This is going to take scientists coming together across disciplines to seek new answers.”
Gewirtz is also working with Chassaing to explore the potential for a vaccine that could inoculate the gut against the havoc caused by a poor diet.
Didier Merlin, professor in the Institute for Biomedical Sciences and a Research Career Scientist at Veteran Affairs Medical Center, is investigating whether a common supermarket ingredient — ginger — could help combat inflammation involved in IBD and colitis-associated colon cancer. A team of researchers led by Merlin is developing ginger-derived nanoparticles to deliver the ingredient’s anti-inflammatory compounds directly to the site of the inflammation.
“It’s a novel, nontoxic delivery system to treat inflamed intestinal tissue,” says Lewins Walter, a Ph.D. candidate and researcher in Merlin’s lab.
“We’re looking at these nanoparticles as a natural remedy for IBD.”
Still, Li notes that overactive inflammation is a complex process with many causes, and finding a solution will require a multipronged approach.
“It won’t be neuroscience or microbiology — or any single science — that will rein in the burden of inflammation or chronic disease,” he says. “This is going to take scientists coming together across disciplines to seek new answers.”










Leave a Reply